MCQ : CHD-07
A 12-Year-Old Boy was found to have a heart murmur and evidence of cardiac enlargement.
What is your diagnosis?
A – Total anomalous pulmonary venous drainage
B – Sinus venosus atrial septal defect with partial anomalous pulmonary venous drainage
C – Pulmonary vein stenosis with partial anomalous pulmonary venous drainage
D – Patent ductus arteriosus with total anomalous pulmonary venous drainage
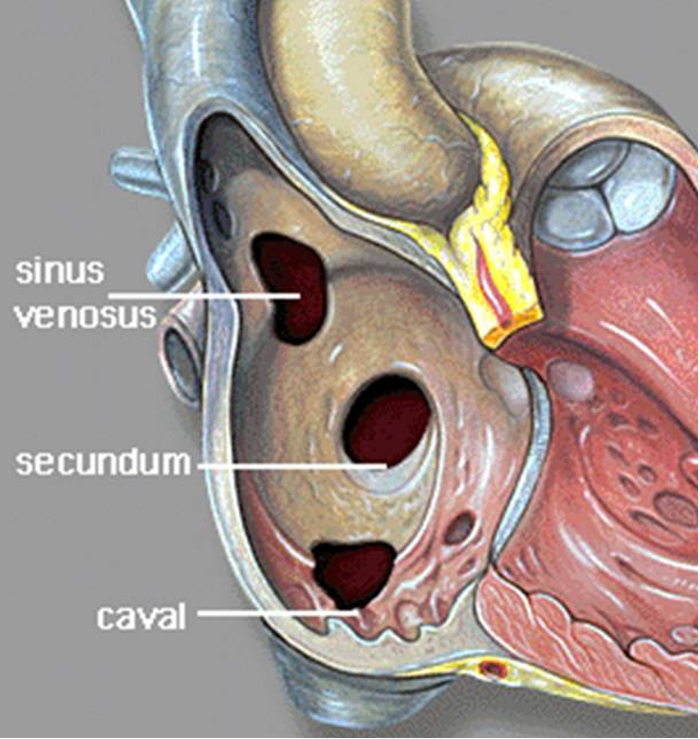
Right answer is B: Sinus venosus atrial septal defect
Sinus venosus atrial septal defects (SVASDs) are rare congenital cardiac abnormalities (5%–10% of all ASDs) that occur at the posterior aspect of the interatrial septum, close to the junction of the superior or inferior vena cava with the right atrium. They involve the portion of the atrial wall that derives from the sinus venosus and they are often associated with partial anomalous pulmonary venous drainage from the right lung. SVASDs result in a left to right shunt at the atrial level, since the left atrial pressure is greater than the right. They may not cause symptoms in childhood, however patients may become symptomatic with ageing. SVASDs have nonspecific clinical manifestations such as exertional dyspnea, arrhythmias, paradoxical embolism. The long term haemodynamic effect is volume overload of the right heart, as a result of the shunt, which can cause pulmonary hypertension if the shunt is significant. Furthermore, the frequently coexistent anomalous pulmonary venous drainage (in around 90% of SVASDs) contributes to additional left-to-right shunting, thus, the development of Eisenmenger physiology can occur earlier compared to an isolated ASD. SVASDs can be misdiagnosed as primary pulmonary hypertension, thus they should always be suspected in case of unexplained right heart chambers dilatation.
![]()